Parents co-sleeping with their infants is a common and accepted practice worldwide. In response to data linking co-sleeping with an increased rate of sudden infant death syndrome, however, the American Academy of Pediatrics since 1992 has recommended that infants share a room but not a bed with their infants. This recent study from the journal JAMA Pediatrics utilizes data from the National Infant Sleep Position study to examine the rates of infant bed sharing from 1993 to 2000 and factors related to the practice.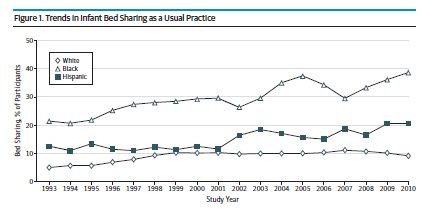
Participants in this study were a national sample of parents (80% mothers) of infants 7 months or younger who were identified from a commercial list and contacted by phone. The final sample of nearly 19,000 individuals was more likely to be Caucasian, older, and well educated compared to national norms. Participation rates varied widely from year to year and generally got worse from 1993 to 2010. Subjects were asked if a parent or guardian usually sleeps with the child. They were also asked if the topic was discussed with their doctor and if the physician’s attitude was positive or negative. The median infant age was about 4.5 months.
Results showed that, 0verall, 11.2% of parents reported that they usually slept with their infant. The prevalence rose 6.5% in 1993 to 13.5% in 2010. Race appeared to be strongly liked with infant bed sharing. In 2010, nearly 40% of black infants slept with a parent compared to just under 10% of white infants. This point was highlighted by the authors as the rate of SIDS is also higher in African American families.
Infant bed sharing was also found to be related to the following factors: lower level of education and income, younger infant age, preterm birth, and geography (higher in the west and south).
Regarding conversations with their doctor, a total of 54% of the sample reported no input from their physician. Of those who did receive advice, nearly three-quarters reported being advised against the practice. Parents who were cautioned against the practice were less likely to share a bed with their child (or perhaps were less likely to admit it).
The authors suggested that more frequent and consistent advice from physicians could help change practices to be more in line with recommendations. An accompanying editorial, however, describes some problems with the data on which these recommendations are made, suggesting that it may be premature to condemn this practice based on the available evidence. It has been suggested that other factors, such as paternal substance use or infant sleeping in other places such as sofas, may be more moderating factors to consider in the link between cosleeping and SIDS.
Reference
Colson E, et al. Trends and Factors Associated With Infant Bed Sharing, 1993-2010: The National Infant Sleep Position Study. JAMA Pediatrics 2013; published online Sept 20.