The New York Times is reporting data they received from the CDC’s National Survey of Children’s Health that the number of children who have received a diagnosis of ADHD has risen to 11% with some segments of the population, such as high school boys, as high as 20%. The data come from phone interviews of over 76,000 parents who participated in this survey that asked about wide ranging health issues. Of note, the Times reports that they received the raw data themselves and compiled these figures. The findings have not been reported in scientific journals or subjected to a peer review process, although the next edition of the Journal of the American Academy of Child and Adolescent Psychiatry is expected to feature an article about the CDC survey.
As would be expected, the report has generated a firestorm of discussion and debate with many concerned that this rise in ADHD diagnosis represents an excessive broadening of the criteria that subjects too many youth needlessly to the dangers associated with ADHD medications. Unfortunately, these data are unable to answer this question. According to the graph accompanying the article, the rate of diagnosed ADHD in Vermont is around the national average.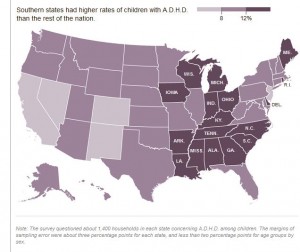
As people debate the important questions raised by this survey, it may be important to keep a few things in mind.
1. ADHD is a real brain-based phenomenon with overwhelming scientific evidence to support its validity.
2. ADHD likely exists more like a continuum (similar to blood pressure or cholesterol) rather than in binary form. Consequently, there is no clear boundary or cut-off between typical and abnormal levels of these behaviors.
3. Establishing a diagnosis of ADHD requires a careful evaluation that includes input from multiple sources and assessment of behaviors relative to expected norms of others of the same age and sex.
4. Family-based multimodal treatment of ADHD can result in substantial improvement but need to be weighed against the potential risks of medications.
Bottom line: Are there kids being diagnosed with ADHD and treated who don’t meet criteria for the diagnosis? Yes. Are these also youth who do meet criteria for ADHD who are suffering needlessly because a lack of diagnosis and treatment? You bet. Let’s work then, to reduce BOTH scenarios and leave the finger pointing to those who don’t have kids to care for.