Dario* is in his 40’s and has been struggling with pain and sleep quality due to the impact of a back injury. Prior to being connected to us, he presented a number of times at the Emergency Department, unaware of where else he could get care. After receiving the exorbitant bills, he was reluctant to go to follow up appointments with the specialists that had been recommended to him. He ultimately was established with a primary care provider who thought physical therapy could be helpful for his pain and long term health but was reluctant to refer him due to high out of pocket costs as an uninsured patient.
Dora* is entering her second trimester of pregnancy and just recently reached out to us about prenatal care options in her area. She is currently ineligible for insurance because, despite only making minimum wage, she and her partner work 132 hours a week to support immediate and extended family members which puts her over the income threshold to qualify. She was charged $260 for the initial visit (equivalent to 21 hours of work at her current hourly rate) and it is recommended that she be seen for 8 more visits leading up to her due date.
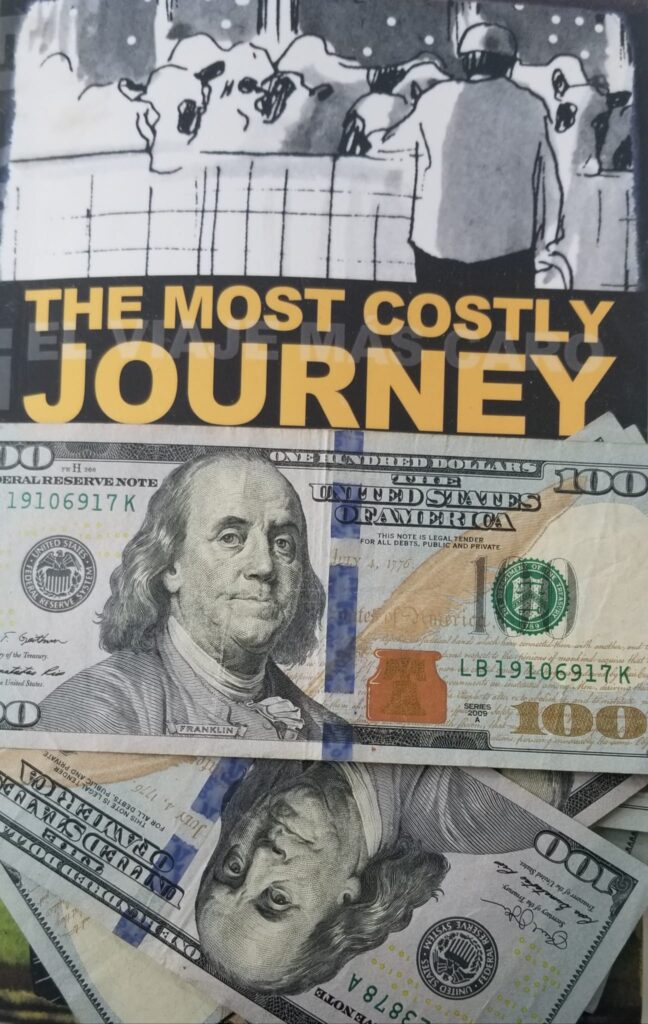
Lina’s* young daughter had worsening and inexplicable pain in a joint. After a series of primary care and specialists appointments, blood work showed significantly elevated levels of white blood cells. After being admitted into the Children’s Hospital, a biopsy and additional blood work, she was diagnosed with a fungal respiratory infection that had entered his blood stream. She was discharged with a prescription for a daily medication that she was to take for a year. When Lina showed up to pick up the prescription she was told that it would be $3000 a month ($36,000 for the year).
Martin* presented at the Emergency Department with severe abdominal pain. They ruled out the need for any emergency procedures and it was recommended he follow up with a specialist for an endoscopy. His initial hospital bill was $5852 with an additional $505 bill from the company the hospital contracts with for diagnostic equipment.
Joseph* is a seasonal agricultural worker with hypertension. He was about to run out of the medication he brought from home and was set up a Community Health Center after 10 weeks of back and forth about whether or not they would see him without him being able to successfully get medical records from home. He was charged $170 for the appointment and his medication that was supposed to be sent to a low cost pharmacy was sent to a local pharmacy instead where it cost over $300 for the month. With a salary of $14.99 an hour, the initial cost of the appointments and meds was more than 32 hours of work in the fields.
Leo* was in a horrific car accident where he was pulled out of the vehicle with the jaws of life. He was brought intermediately by ambulance to the trauma center at a Vermont hospital where he was admitted for over a month incurring over a hundred thousand dollars of health related costs.
In all of the above scenarios, there are opportunities to reduce the price of care that the individuals and families did not know about and in all of these cases, health care system representatives either did not explain, did not explain in a language that the patient understood, or did not know about ways to reduce the out of pocket cost. Dario was eligible for financial assistance at the hospital which means that he is eligible for discounted care at physical therapists that are within the hospital system. Dora was eligible for a 30% self-pay discount for her prenatal visits. Lina’s insurance covers the cost of her medications as long as the provider submits evidence of need for pre-approval. Martin, with a wife and three minor children was eligible for financial assistance at the hospital and if he sends in the approval letter, the diagnostic imagining company will provide a discount as well. Joseph had been incorrectly assessed for the slide fee discount and was eligible for a refund for the provider visit (unfortunately he couldn’t recoup the costs of the medications). Leo was eligible for Emergency Medicaid given his inability to work after the accident which covered the cost of his in-patient care.
In each of these cases, due to extensive outreach and an unwavering commitment to improving access to care for migrant workers and their family members living in Vermont, Bridges to Health either had pre-established relationships with those impacted or a friend, family member, or employer referred them to us. We were able to assist in each one of the above cases to reduce the out of pocket health care costs and support needed follow up care because we have a unique understanding of the individual and systems barriers faced by migrant workers and their family members as well as years of experience navigating similar cases. The cost of care is an issue that we confront with clients on a weekly basis and is often cited as a reason that they have delayed or forgone needed care until their health deteriorates significantly.
It is clear from these cases and the hundreds that we have worked on over the years, that hospitals and health centers are not giving migrant workers and their family members adequate information about or support to navigate the complex and confusing payment, financial assistance, and health insurance systems. How does this impact decisions about preventative care or seeking out needed care in a timely manner? How many cancel or skip appointments or forgo costly prescriptions? What would be the long term costs to both personal health and the health care system if Dario ended up back in the ED when his back pain gets worse, Martin doesn’t get the endoscopy, Joseph rationed his blood pressure medication, Lina’s daughter went without treatment or Dora didn’t get prenatal care? How many more are getting lost in the health care costs labyrinth?