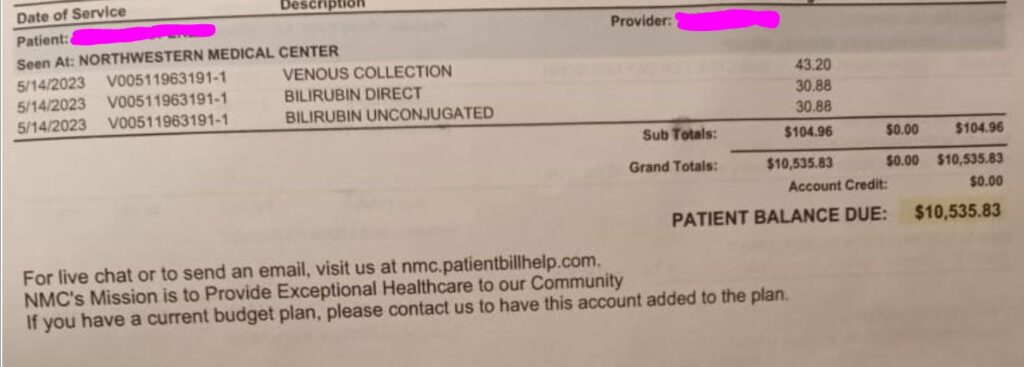
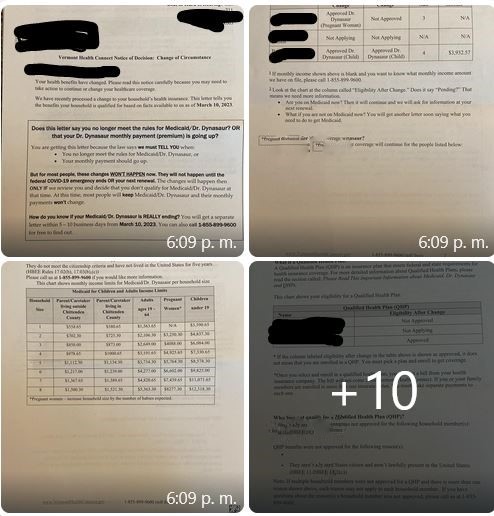
Elisa reached out this week after receiving a bill in her name for over $200 and a final reminder notice on a bill in her mom’s name of over $400. She was perplexed, as was I, since we submitted a sliding fee application for the family along with registration paperwork back in October prior to making their appointments and been told that the family would just have to pay a nominal fee. Since the first bills started to arrive, we had followed up on two prior occasions and been told the clinic’s sliding fee had been incorrectly processed and both times we had been assured it would be remedied. With yet another round of bills, we hopped on a three way call with billing at the clinic so I could interpret and explained the situation. In the case of Elisa’s bill, we explained we had received an email over a month ago confirming that the bill would be reprocessed and the amount lowered. In the case of the mom, the clinic had no record on the account that the sliding fee had been added to her account. The billing representative reviewed the notes and said “looks like some stuff got missed.” She sent an email off to the folks who handle the financial assistance applications and told us we would be hearing from someone soon. We are still waiting and in the meantime I am trying to assure the family, who has no income while they navigate the asylum seeking process, not to stress out, to have faith in a system that requires at least three calls to fix a mistake that without a correction will put the family on a debt collectors list.
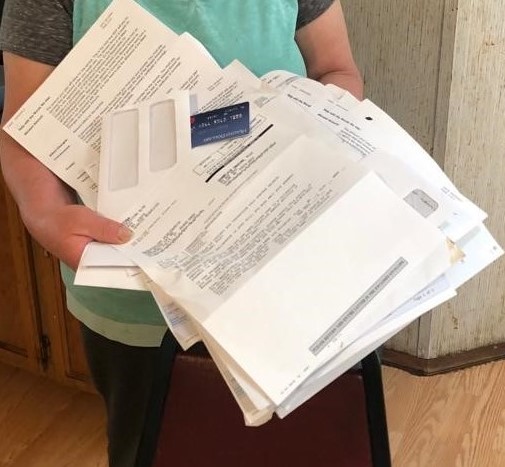
If this was just occasional call that we have to make together with clients to fix billing errors, maybe it wouldn’t feel like such a big deal. People are overworked, they make mistakes, stuff gets missed. But we spend an obscene amount of time calling about bills that we have already called about that should have been resolved and resubmitting paperwork that we already submitted because despite being submitted as a complete application it somehow got misplaced or separated from the account in question. For as many cases as we help clients resolve, I can only imagine how many more mistakes go unfixed or unnoticed. And for most of our clients, the whole process of billing and applying for financial assistance or health insurance is an unfamiliar process made even more challenging to navigate when there is a language barrier as well as work schedules in service industries that often make it impossible to make a call to a clinic during normal business hours. For our team, what makes this time spent on resolving payments even more frustrating is that there are so many people who request our support to navigate access to needed health care services who we could be helping if we weren’t on the phone buried under the health care systems administrative burden.